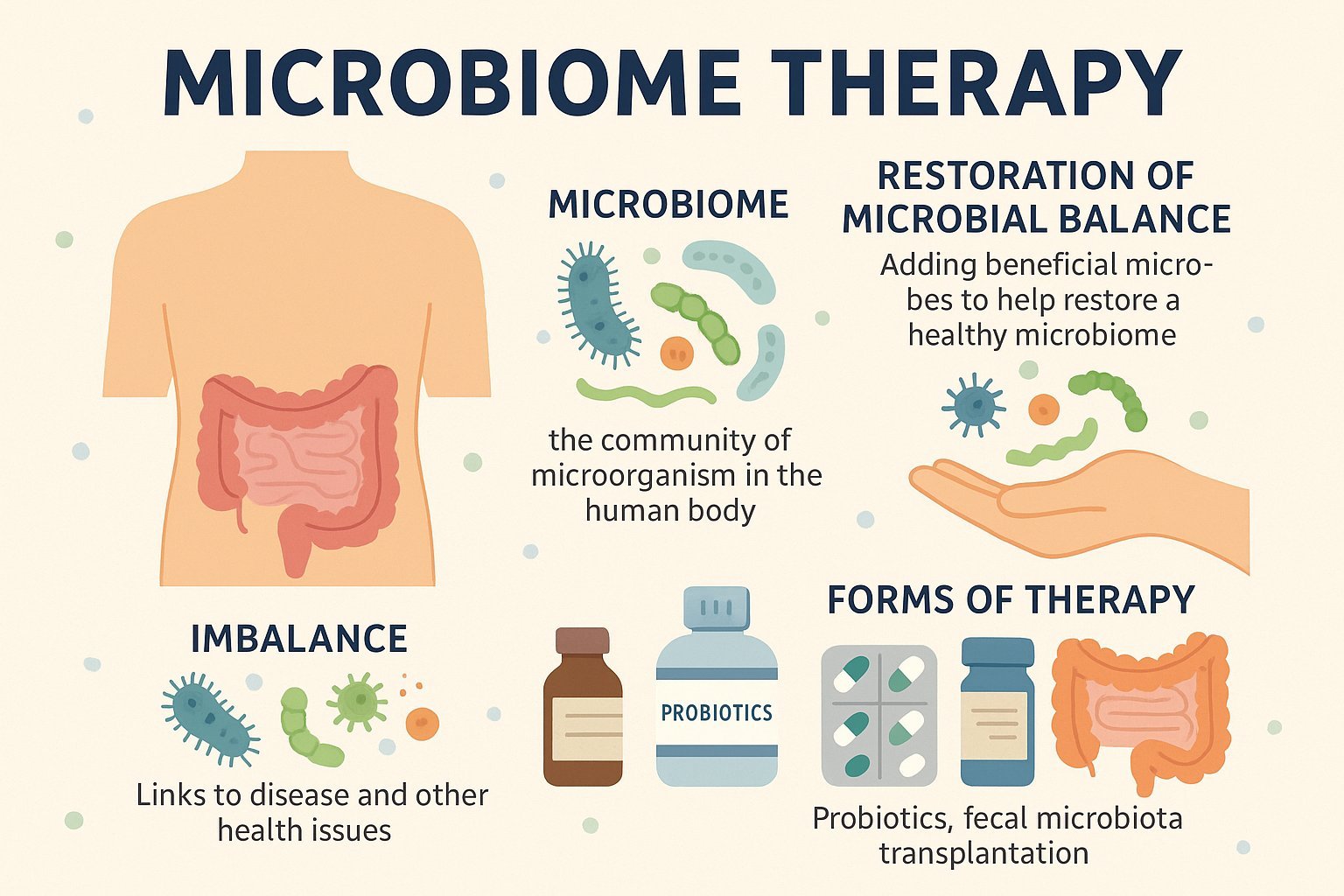
Inside the human body lives a hidden world of trillions of microorganisms. They occupy the skin, mouth, and especially the gut, forming what scientists call the microbiome. For decades, medicine often saw microbes mainly as threats, linked to infections and disease. But recent discoveries show that most of these tiny life forms are actually vital allies. They help us digest food, shape our immune system, and even influence our mental health. Out of this understanding has grown a new approach in medicine known as microbiome therapy, an effort to use these natural companions as a form of treatment.
Understanding the Microbiome
The microbiome is the collection of bacteria, fungi, viruses, and other microorganisms that live in and on the body. The gut microbiome has drawn the most attention because of its impact on digestion, nutrient absorption, and immunity. A healthy balance of microbes supports overall wellness, but disruptions caused by antibiotics, illness, or poor diet can disturb this balance. When that happens, problems such as chronic digestive disorders, allergies, obesity, and even anxiety or depression may appear.
The Idea of Microbiome Therapy
The central idea of microbiome therapy is simple: if the balance of microbes is disturbed, it can be restored by introducing helpful ones. Rather than relying solely on chemical drugs, this approach uses living organisms that are naturally part of the body’s ecosystem. In many ways, it resembles gardening—replacing weeds with strong, healthy plants until the environment thrives again.
How It Works in the Body
Beneficial microbes play many roles in keeping us healthy. They break down complex fibers from food into short-chain fatty acids, which fuel intestinal cells and reduce inflammation. They produce substances that influence immunity, helping the body respond to threats without overreacting. Some even send signals to the brain through what scientists call the gut–brain axis, linking digestive health with mood and cognition. By restoring microbial communities, microbiome therapy reactivates these natural pathways of support.
Challenges Facing the Field
Although the potential is exciting, microbiome therapy is still developing. Every individual’s microbiome is unique, shaped by genetics, environment, and lifestyle. What works for one person may not work for another. Safety is another concern. Introducing living organisms must be done with care to avoid unexpected side effects. Scientists also continue to study which microbial combinations are the most beneficial and how long their effects last.
Approaches to Microbiome Therapy
One familiar form of microbiome-based treatment is the use of probiotics. These are live microbes, commonly from groups such as Lactobacillus and Bifidobacterium, taken in foods, drinks, or capsules. Probiotics have already become widely available, but medical research is exploring more precise therapies. Another approach is fecal microbiota transplantation (FMT). Though it may sound unusual, it has shown remarkable success in treating serious gut infections, particularly those caused by Clostridioides difficile. In FMT, stool from a healthy donor is transplanted into a patient’s intestine, transferring a robust community of microbes that can restore balance.
Researchers are also developing targeted therapies involving carefully selected bacterial strains. Early studies suggest that some microbes could help manage inflammatory bowel disease, metabolic conditions like diabetes, or even neurological disorders. These treatments are still experimental, but they hint at a future where doctors could prescribe microbes as confidently as they prescribe medicines today.
The Road Ahead
Despite these hurdles, progress is moving quickly. Clinical trials are under way to test therapies for conditions ranging from autoimmune diseases to cancer. With advances in genetic sequencing and microbial science, the possibility of personalized microbiome treatments is becoming more realistic. In the coming years, doctors may be able to design therapies tailored to the specific microbial patterns of each patient.
Why It Matters
The study of the microbiome has changed the way health is understood. Instead of viewing microbes only as invaders, medicine now recognizes them as partners. Microbiome therapy represents a natural way of restoring balance rather than fighting the body’s systems. It offers hope not only for difficult-to-treat infections but also for long-term conditions that conventional drugs struggle to manage.
Microbiome therapy is opening a new chapter in medicine. By working with the microorganisms that already live within us, this field offers the possibility of safer, more natural, and more effective treatments. Much remains to be learned, but the progress so far suggests that our smallest companions may hold the key to some of the greatest medical advances of the future.